Edition: BP 2025 (Ph. Eur. 11.6 update)
Action and use
Cyclo-oxygenase inhibitor; analgesic; anti-inflammatory.
Preparations
Naproxen Oral Suspension Naproxen Tablets
Naproxen Gastro-resistant Tablets Ph Eur
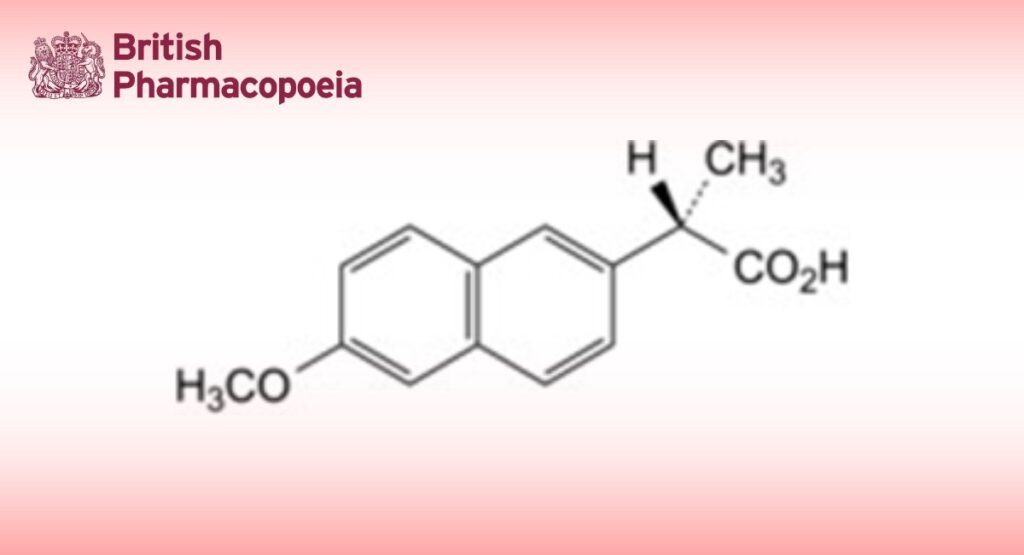
DEFINITION
(2S)-2-(6-Methoxynaphthalen-2-yl)propanoic acid.
Content
99.0 per cent to 101.0 per cent (dried substance).
CHARACTERS
Appearance
White or almost white, crystalline powder.
Solubility
Practically insoluble in water, soluble in ethanol (96 per cent) and in methanol.
IDENTIFICATION
First identification: A, D.
Second identification: A, B, C.
A. Specific optical rotation (2.2.7): + 59 to + 62 (dried substance).
Dissolve 0.50 g in ethanol (96 per cent) R and dilute to 25.0 mL with the same solvent.
B. Melting point (2.2.14): 154 °C to 158 °C.
C. Ultraviolet and visible absorption spectrophotometry (2.2.25).
Test solution Dissolve 40.0 mg in methanol R and dilute to 100.0 mL with the same solvent. Dilute 10.0 mL of the solution to 100.0 mL with methanol R.
Spectral range 230-350 nm.
Absorption maxima At 262 nm, 271 nm, 316 nm and 331 nm.
Specific absorbances at the absorption maxima:
— at 262 nm: 216 to 238;
— at 271 nm: 219 to 241;
— at 316 nm: 61 to 69;
— at 331 nm: 79 to 87.
D. Infrared absorption spectrophotometry (2.2.24).
Comparison naproxen CRS.
TESTS
Appearance of solution
The solution is clear (2.2.1) and not more intensely coloured than reference solution BY7 (2.2.2, Method II). Dissolve 1.25 g in methanol R and dilute to 25 mL with the same solvent.
Enantiomeric purity
Liquid chromatography (2.2.29). Protect the solutions from light.
Test solution Dissolve 25.0 mg of the substance to be examined in tetrahydrofuran R and dilute to 50.0 mL with the same solvent. Dilute 2.0 mL of the solution to 20.0 mL with the mobile phase.
Reference solution (a) Dilute 2.5 mL of the test solution to 100.0 mL with the mobile phase.
Reference solution (b) Dissolve 5 mg of racemic naproxen CRS in 10.0 mL of tetrahydrofuran R and dilute to 100.0 mL with the mobile phase.
Column:
— size: l = 0.25 m, Ø = 4.6 mm;
— stationary phase: silica gel π-acceptor/π-donor for chiral separations R (5 µm) (S,S);
— temperature: 25 °C.
Mobile phase glacial acetic acid R, acetonitrile R, 2-propanol R, hexane R (0.5:5:10:84.5 V/V/V/V). Flow rate 2 mL/min.
Detection Spectrophotometer at 263 nm.
Injection 20 µL.
Run time 1.5 times the retention time of naproxen (retention time = about 5 min).
System suitability Reference solution (b):
— resolution: minimum 3 between the peaks due to impurity G and naproxen.
Limit:
— impurity G: not more than the area of the principal peak in the chromatogram obtained with reference solution (a) (2.5 per cent).
Related substances
Liquid chromatography (2.2.29). Protect the solutions from light.
Test solution Dissolve 12 mg of the substance to be examined in the mobile phase and dilute to 20 mL with the mobile phase.
Reference solution (a) Dilute 1.0 mL of the test solution to 50.0 mL with the mobile phase. Dilute 1.0 mL of this solution to 20.0 mL with the mobile phase.
Reference solution (b) Dissolve 6 mg of bromomethoxynaphthalene R (impurity N), 6.0 mg of naproxen impurity L CRS, 6 mg of 6-methoxy-2-naphthoic acid R (impurity O) and 6 mg of (1RS)-1-(6-methoxynaphthalen-2-yl)ethanol R (impurity K) in acetonitrile R and dilute to 10.0 mL with the same solvent. To 1.0 mL of the solution add 1.0 mL of the test solution and dilute to 50.0 mL with the mobile phase. Dilute 1.0 mL of this solution to 20.0 mL with the mobile phase.
Column:
— size: l = 0.10 m, Ø = 4.0 mm;
— stationary phase: end-capped octadecylsilyl silica gel for chromatography R (3 µm);
— temperature: 50 °C.
Mobile phase Mix 42 volumes of acetonitrile R and 58 volumes of a 1.36 g/L solution of potassium dihydrogen phosphate R previously adjusted to pH 2.0 with phosphoric acid R.
Flow rate 1.5 mL/min.
Detection Spectrophotometer at 230 nm.
Injection 20 µL.
Run time 1.5 times the retention time of impurity N.
Identification of impurities Use the chromatogram obtained with reference solution (b) to identify the peaks due to impurities K, L, N and O.
Relative retention With reference to naproxen (retention time = about 2.5 min): impurity O = about 0.8; impurity K = about 0.9; impurity L = about 1.4; impurity N = about 5.3.
System suitability Reference solution (b):
— resolution: minimum 2.2 between the peaks due to impurity K and naproxen.
Limits:
— correction factor: for the calculation of content, multiply the peak area of impurity O by 2.0;
— impurity O: not more than 1.5 times the area of the principal peak in the chromatogram obtained with reference solution (a) (0.15 per cent);
— impurity L: not more than 1.5 times the area of the corresponding peak in the chromatogram obtained with reference solution (b) (0.15 per cent);
— unspecified impurities: for each impurity, not more than the area of the principal peak in the chromatogram obtained with reference solution (a) (0.10 per cent);
— total: not more than 3 times the area of the principal peak in the chromatogram obtained with reference solution (a) (0.3 per cent);
— disregard limit: 0.5 times the area of the principal peak in the chromatogram obtained with reference solution (a) (0.05 per cent).
Loss on drying (2.2.32)
Maximum 0.5 per cent, determined on 1.000 g by drying in an oven at 105 °C for 3 h.
Sulfated ash (2.4.14)
Maximum 0.1 per cent, determined on 1.0 g.
ASSAY
Dissolve 0.200 g in a mixture of 25 mL of water R and 75 mL of methanol R. Titrate with 0.1 M sodium hydroxide, using 1 mL of phenolphthalein solution R as indicator.
1 mL of 0.1 M sodium hydroxide is equivalent to 23.03 mg of C14H14O3.
STORAGE
Protected from light.
IMPURITIES
Specified impurities G, L, O.
Other detectable impurities (the following substances would, if present at a sufficient level, be detected by one or other of the tests in the monograph. They are limited by the general acceptance criterion for other/unspecified impurities and/or by the general monograph Substances for pharmaceutical use (2034). It is therefore not necessary to identify these impurities for demonstration of compliance. See also 5.10.
Control of impurities in substances for pharmaceutical use) A, B, C, D, E, F, H, I, J, K, M, N.
A. (2S)-2-(6-hydroxynaphthalen-2-yl)propanoic acid,
B. (2S)-2-(5-chloro-6-methoxynaphthalen-2-yl)propanoic acid,
C. (2S)-2-(5-bromo-6-methoxynaphthalen-2-yl)propanoic acid,
D. (2S)-2-(5-iodo-6-methoxynaphthalen-2-yl)propanoic acid,
E. methyl (2S)-2-(6-methoxynaphthalen-2-yl)propanoate,
F. ethyl (2S)-2-(6-methoxynaphthalen-2-yl)propanoate,
G. (2R)-2-(6-methoxynaphthalen-2-yl)propanoic acid ((R)-enantiomer),
H. 6-methoxynaphthalen-2-ol,
I. (6-methoxynaphthalen-2-yl)acetic acid,
J. 2-ethyl-6-methoxynaphthalene,
K. (1RS)-1-(6-methoxynaphthalen-2-yl)ethanol,
L. 1-(6-methoxynaphthalen-2-yl)ethanone,
M. 2-methoxynaphthalene (nerolin),
N. 2-bromo-6-methoxynaphthalene,
O. 6-methoxynaphthalene-2-carboxylic acid (6-methoxy-2-naphthoic acid).
Ph Eur