(Ph. Eur. monograph 0179)
Action and use
Macrolide antibacterial.
Preparations
Erythromycin Gastro-resistant Capsules
Erythromycin Gastro-resistant Tablets
Erythromycin and Zinc Acetate Lotion
DEFINITION
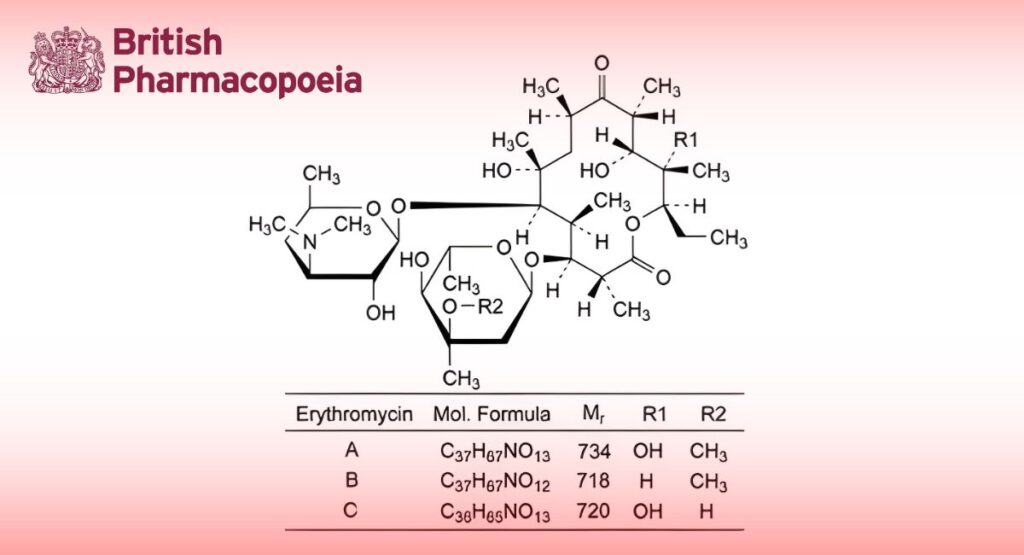
Mixture of macrolide antibiotics produced by a strain of Streptomyces erythreus.
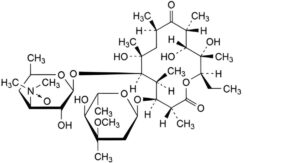
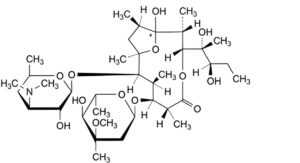
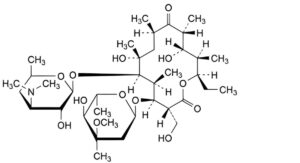
Main component (3R,4S,5S,6R,7R,9R,11R,12R,13S,14R)-4-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-14-ethyl-7,12,13-trihydroxy-3,5,7,9,11,13-hexamethyl-6-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-1-oxacyclotetradecane-2,10-dione (erythromycin A).
Content
— sum of erythromycins A, B and C: 93.0 per cent to 102.0 per cent (anhydrous substance);
— erythromycin B: maximum 5.0 per cent (anhydrous substance);
— erythromycin C: maximum 5.0 per cent (anhydrous substance).
CHARACTERS
Appearance
White or slightly yellow powder or colourless or slightly yellow crystals, slightly hygroscopic.
Solubility
Slightly soluble in water (the solubility decreases as the temperature rises), freely soluble in ethanol (96 per cent), soluble in methanol.
It shows polymorphism (5.9).
IDENTIFICATION
First identification: A.
Second identification: B.
A. Infrared absorption spectrophotometry (2.2.24).
Comparison: erythromycin A CRS.
Disregard any band in the region from 1980 cm to 2050 cm .
If the spectra obtained show differences, dissolve 50 mg of the substance to be examined and of the reference substance separately in 1.0 mL of methylene chloride R, dry in vacuo at 60 °C for 3 h at a pressure not exceeding 0.7 kPa and record new spectra using the residues.
B. Thin-layer chromatography (2.2.27).
Test solution: Dissolve 10 mg of the substance to be examined in methanol R and dilute to 10 mL with the same solvent.
Reference solution (a): Dissolve 10 mg of erythromycin A CRS in methanol R and dilute to 10 mL with the same solvent.
Reference solution (b): Dissolve 20 mg of spiramycin CRS in methanol R and dilute to 10 mL with the same solvent.
Plate: TLC silica gel plate R.
Mobile phase: Mix 4 volumes of 2-propanol R, 8 volumes of a 150 g/L solution of ammonium acetate R previously
adjusted to pH 9.6 with ammonia R, and 9 volumes of ethyl acetate R; allow to settle and use the upper layer.
Application: 10 μL.
Development: Over 2/3 of the plate.
Drying: In air.
Detection: Spray with anisaldehyde solution R1 and heat at 110 °C for 5 min.
Results: The principal spot in the chromatogram obtained with the test solution is similar in position, colour and size to the principal spot in the chromatogram obtained with reference solution (a), and its position and colour are different from those of the spots in the chromatogram obtained with reference solution (b).
TESTS
Related substances
Liquid chromatography (2.2.29). Prepare the solutions immediately before use.
Solution A: Dissolve 11.5 g of dipotassium hydrogen phosphate R in 900 mL of water R, adjust to pH 8.0 with dilute phosphoric acid R and dilute to 1000 mL with water R.
Solvent mixture: methanol R, solution A (40:60 V/V).
Test solution: Dissolve 40.0 mg of the substance to be examined in the solvent mixture and dilute to 10.0 mL with the solvent mixture.
Reference solution (a): Dissolve 40.0 mg of erythromycin A CRS in the solvent mixture and dilute to 10.0 mL with the solvent mixture.
Reference solution (b): Dissolve 10.0 mg of erythromycin B CRS and 10.0 mg of erythromycin C CRS in the solvent mixture and dilute to 50.0 mL with the solvent mixture.
Reference solution (c): Dilute 1.0 mL of reference solution (a) to 100.0 mL with the solvent mixture.
Reference solution (d): Dissolve 4 mg of erythromycin for system suitability CRS (containing impurities A, B, C, D, E, F, H and L) in the solvent mixture and dilute to 1 mL with the solvent mixture.
Column:
— size: l = 0.25 m, Ø = 4.6 mm;
— stationary phase: end-capped polar-embedded octadecylsilyl amorphous organosilica polymer R (3.5 μm);
— temperature: 65 °C; preheating the mobile phase may be required, for instance by extending the inlet tubing in the oven to 30 cm.
Mobile phase:
— mobile phase A: phosphate buffer solution pH 7.0 R7, acetonitrile R1, water for chromatography R (5:35:60 V/V/V);
— mobile phase B: phosphate buffer solution pH 7.0 R7, water for chromatography R, acetonitrile R1 (5:45:50 V/V/V);
| Time (min) |
Mobile phase A (per cent V/V) |
Mobile phase B (per cent V/V) |
| 0 – tR | 100 | 0 |
| tR – (tR + 2) | 100 → 0 | 0 → 100 |
| (tR + 2) – (tR + 15) | 0 | 100 |
tR = retention time of erythromycin B, determined by injecting 10 μL of reference solution (b) and eluting with mobile phase A.
Flow rate: 1.0 mL/min.
Detection: Spectrophotometer at 210 nm.
Autosampler: Set at 4 °C.
Injection: 100 μL of the test solution and reference solutions (b), (c) and (d).
Identification of impurities: Use the chromatogram supplied with erythromycin for system suitability CRS and the chromatogram obtained with reference solution (d) to identify the peaks due to impurities A, B, C, D, E, F, H and L; use the chromatogram obtained with reference solution (b) to identify the peaks due to erythromycins B and C.
Relative retention: With reference to erythromycin A (retention time = about 23 min): impurity H = about 0.3; impurity A = about 0.4; impurity B = about 0.5; erythromycin C = about 0.55; impurity L = about 0.63; impurity C = about 0.9; impurity D = about 1.61; erythromycin B = about 1.75; impurity F = about 1.81; impurity E = about 2.3.
System suitability: Reference solution (d):
— resolution: minimum 1.2 between the peaks due to impurity B and erythromycin C;
— peak-to-valley ratio: minimum 1.5, where Hp = height above the baseline of the peak due to impurity F and
Hv = height above the baseline of the lowest point of the curve separating this peak from the peak due to erythromycin B; minimum 2.0, where Hp = height above the baseline of the peak due to impurity C and Hv = height above the baseline of the lowest point of the curve separating this peak from the peak due to erythromycin
A. If necessary, adjust the concentration of acetonitrile in the mobile phases and/or the gradient to obtain the required separation.
Calculation of percentage contents:
— correction factors: multiply the peak areas of the following impurities by the corresponding correction factor:
impurity D = 2; impurity E = 0.08; impurity F = 0.08; impurity L = 0.11;
— for each impurity, use the concentration of erythromycin A in reference solution (c).
Limits:
— impurity C: maximum 3.0 per cent;
— impurities A, B: for each impurity, maximum 2.0 per cent;
— impurities D, E, F, H: for each impurity, maximum 1.0 per cent;
— impurity L: maximum 0.4 per cent;
— any other impurity: for each impurity, maximum 0.4 per cent;
— total: maximum 7.0 per cent;
— reporting threshold: 0.2 per cent; disregard the peaks due to erythromycins B and C.
Thiocyanate
Maximum 0.3 per cent.
Prepare the solutions immediately before use and protect from actinic light.
Compensation liquid: Dilute 1.0 mL of a 90 g/L solution of ferric chloride R to 50.0 mL with methanol R.
Test solution Dissolve 0.100 g of the substance to be examined in 20 mL of methanol R, add 1.0 mL of a 90 g/L solution of ferric chloride R and dilute to 50.0 mL with methanol R.
Prepare 2 independent reference solutions.
Reference solution: Dissolve 0.100 g of potassium thiocyanate R, previously dried at 105 °C for 1 h, in methanol R and dilute to 50.0 mL with the same solvent. Dilute 5.0 mL of the solution to 50.0 mL with methanol R. To 5.0 mL of this solution, add 1.0 mL of a 90 g/L solution of ferric chloride R and dilute to 50.0 mL with methanol R.
Measure the absorbance (2.2.25) of each reference solution (A1, A2) and of the test solution (A) at the absorption maximum (about 492 nm).
Suitability value:
m1, m2 = mass of potassium thiocyanate used to prepare reference solutions A1 and A2 respectively, in grams.
The test is not valid unless S is not less than 0.985 and not greater than 1.015.
Calculate the percentage content of thiocyanate using the following expression:
m = mass of the substance to be examined used to prepare the test solution, in grams;
58.08 = relative molecular mass of the thiocyanate moiety;
97.18 = relative molecular mass of potassium thiocyanate.
Water (2.5.12)
Maximum 6.5 per cent, determined on 0.200 g.
Use a 100 g/L solution of imidazole R in anhydrous methanol R as the solvent.
Sulfated ash (2.4.14)
Maximum 0.2 per cent, determined on 1.0 g.
ASSAY
Liquid chromatography (2.2.29) as described in the test for related substances with the following modifications.
Injection: Test solution and reference solutions (a) and (b).
System suitability: Reference solution (a):
— symmetry factor: maximum 2.5 for the peak due to erythromycin A;
— repeatability: maximum relative standard deviation of 1.0 per cent determined on 6 injections.
Calculate the percentage content of erythromycin A (C37H67NO13) using the chromatogram obtained with reference solution (a). Calculate the percentage contents of erythromycin B (C37H67NO12) and erythromycin C (C36H65NO13) using the chromatogram obtained with reference solution (b).
STORAGE
In an airtight container, protected from light.
IMPURITIES
Specified impurities A, B, C, D, E, F, H, L.
Other detectable impurities (the following substances would, if present at a sufficient level, be detected by one or other of the tests in the monograph. They are limited by the general acceptance criterion for other/unspecified impurities. It is therefore not necessary to identify these impurities for demonstration of compliance. See also 5.10. Control of impurities in substances for pharmaceutical use) I, J, K, M, N.
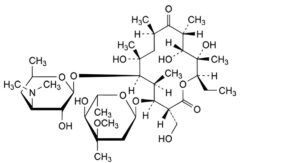
A. (3R,4S,5S,6R,7R,9R,11R,12R,13S,14R)-4-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-14-ethyl- 7,12,13-trihydroxy-3-(hydroxymethyl)-5,7,9,11,13-pentamethyl-6-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo- hexopyranosyl]oxy]-1-oxacyclotetradecane-2,10-dione (erythromycin F),
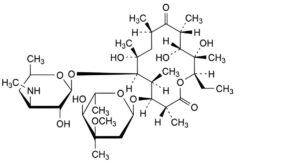
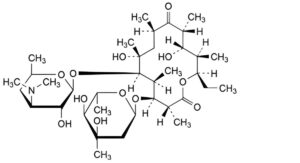
B. (3R,4S,5S,6R,7R,9R,11R,12R,13S,14R)-4-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-14-ethyl- 7,12,13-trihydroxy-3,5,7,9,11,13-hexamethyl-6-[[3,4,6-trideoxy-3-(methylamino)-β-D-xylo-hexopyranosyl]oxy]-1- oxacyclotetradecane-2,10-dione (3′′-N-demethylerythromycin A),
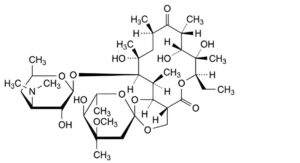
C. (2S,4aR,4′R,5′S,6′S,7R,8S,9R,10R,12R,14R,15R,16S,16aS)-7-ethyl-5′,8,9,14-tetrahydroxy-4′-methoxy-4′,6′,8,10,12,14,16-heptamethyl-15-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-exopyranosyl]oxy]-4,4a,7,8,9,10,12,13,14,15,16,16a-dodecahydro-5H,11H-spiro[[1,3]dioxino[5,4-c][1]oxacyclotetradecin-2,2′-oxane]-5,11-dione (erythromycin E),
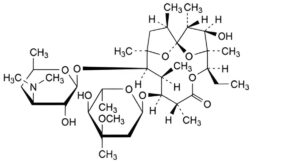
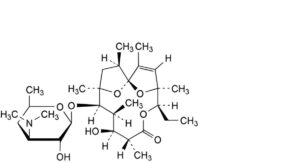
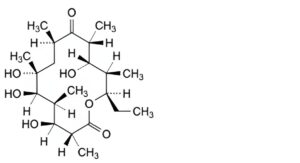
D. (1S,2R,3R,4S,5R,8R,9S,10S,11R,12R,14R)-9-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-5-ethyl-3-hydroxy-2,4,8,10,12,14-hexamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-6,15,16-trioxatricyclo[10.2.1.1 ]hexadecan-7-one (anhydroerythromycin A), 1,4
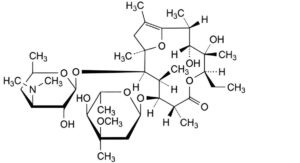
E. (1 R,2R,3R,4S,5R,8R,9S,10S,11R)-9-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-5-ethyl-3,4- dihydroxy-1 ,1 ,2,4,8,10-hexamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-1 ,1 -dihydro-6- oxa-1(2,5)-furanacycloundecaphan-7-one (erythromycin A enol ether),
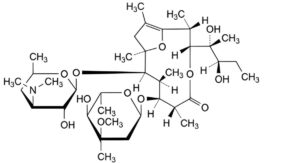
F. (1 R,2R,3R,6R,7S,8S,9R)-7-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-3-[(2R,3R)-2,3-dihydroxypentan-2-yl]-1 ,1 ,2,6,8-pentamethyl-9-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-1 ,1 – dihydro-4-oxa-1(2,5)-furanacyclononaphan-5-one (pseudoerythromycin A enol ether),
H. (3R,4S,5S,6R,7R,9R,11R,12R,13S,14R)-4-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-14- ethyl-7,12,13-trihydroxy-3,5,7,9,11,13-hexamethyl-2,10-dioxo-1-oxacyclotetradecan-6-yl 3,4,6-trideoxy-3-(dimethylamino)- β-D-xylo-hexopyranoside N-oxide (erythromycin A 3′′-N-oxide),
I. (1S,4S,5R,8R,9S,10S,11R,12R,14R)-5-ethyl-9-hydroxy-2,4,8,10,12,14-hexamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-6,15,16-trioxatricyclo[10.2.1.1 ]hexadec-2-en-7-one (erythralosamine),
J. (1RS,2R,3R,6R,7S,8S,9R,10R,12R)-7-[(2,6-dideoxy-3-[(2R,3R)-2,3-dihydroxypentan-2-yl]-1-hydroxy-2,6,8,10,12- pentamethyl-9-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-4,13-dioxabicyclo[8.2.1]tridecan-5-one (pseudoerythromycin A hemiketal),
K. (3R,4S,5S,6R,7R,9R,11R,12S,13R,14R)-4-[(2,6-dideoxy-3-C-methyl-α-L-ribo-hexopyranosyl)oxy]-14-ethyl-7,12- dihydroxy-3,5,7,9,11,13-hexamethyl-6-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-1-oxacyclotetradecane-2,10-dione (erythromycin D),
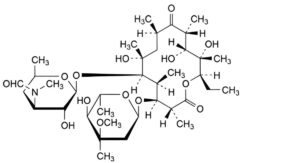
L. (3R,4S,5S,6R,7R,9R,11R,12R,13S,14R)-4-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-14-ethyl- 7,12,13-trihydroxy-3,5,7,9,11,13-hexamethyl-6-[[3,4,6-trideoxy-3-[formyl(methyl)amino]-β-D-xylo-hexopyranosyl]oxy]-1- oxacyclotetradecane-2,10-dione (3′′-N-demethyl-3′′-N-formyl erythromycin A),
M. (3R,4S,5S,6R,7R,9R,11R,12S,13R,14R)-4-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-14- ethyl-7,12-dihydroxy-3-(hydroxymethyl)-5,7,9,11,13-pentamethyl-6-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo- hexopyranosyl]oxy]-1-oxacyclotetradecane-2,10-dione (erythromycin G),
N. (3R,4S,5S,6R,7R,9R,11R,12S,13R,14R)-14-ethyl-4,6,7,12-tetrahydroxy-3,5,7,9,11,13-hexamethyl-1-
oxacyclotetradecane-2,10-dione (erythronolide B).